This job aid outlines the process for a Benefits Partner to add Medicare information such as the Medicare Beneficiary Identifier (MBI) number and enrollment dates.
Managing Medicare Information for Your Employee

Important Information
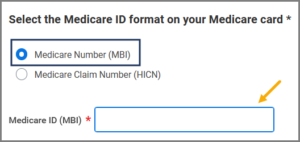
- All Medicare participants should have received a new card with an MBI number (to replace the previous Health Insurance Claim Number [HICN]). If you have an Employee or Retiree who has not received an MBI, they should contact 1‑800‑MEDICARE (1-800-633-4227). You must provide the MBI when adding Medicare information for Employees and Retirees and their Dependents, if applicable.
- Ensure you are not waiting on benefit enrollment until the Medicare card is received for Retirees. They should remain in A&M Care until they have provided the Medicare card (with A&B enrollment). Then they can switch to the 65+ plan on the 1st of the following month. Do not make retroactive enrollment changes. This will cause issues with our EGWP/Medicare Part D process.
- Do not enroll an individual in 65+ if they still plan on working in a benefit eligible position currently or in the future. Only move them to the 65+ plan when they are permanently retired. They should stay in the RAAMP plan or A&M Care while they are still a working retiree.
- Recommendation: Add this to your off-boarding/retirement process to discuss with your Retirees during retirement benefit counseling.
Getting Started
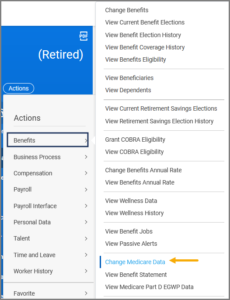
Add or Edit Medicare Information
Note: Alternatively, you can search for Manage Medicare Information in the Search bar and enter the Employee UIN or Name.
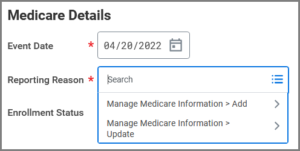
- Under the Medicare Details section, enter the Event Date and Reporting Reason.
IMPORTANT: Do not select the Medicare Claim Number (HICN) button. HICNs are no longer used by the Federal Government.
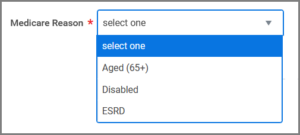
- For the Medicare Reason, select one:
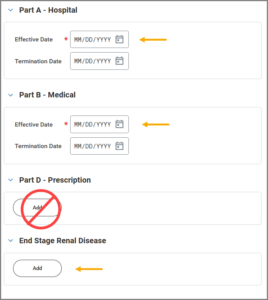
- Complete Parts A & B (and ESRD, if needed). In most cases the Effective Date is the first day of the Employee or Retiree’s birthday month.
IMPORTANT: Leave Part D blank as Medicare prescription enrollment is handled separately.
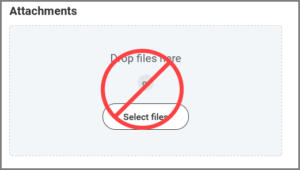
IMPORTANT: Do not attach or upload files on this screen. Medical documentation and other sensitive information are kept separate from Workday.
- Enter any Comments, as needed.
- Select Submit.
Up Next
To Do: Initiate Medical Change Only Benefit Event (Initiator)
The Benefits Partner may receive a To Do to initiate a Medical Change Only Benefit Event. Be Advised: When updating Medicare for a Dependent only, a Medical Change Only benefit event will not trigger for a Dependent as they remain under the Employee or Retiree coverages.
- Follow the instructions in the To Do. If a Medical Change Only benefit event is needed, you must use same Event Date you used for the Manage Medicare process; therefore, it is very important to use the CURRENT date (and not a retroactive date).
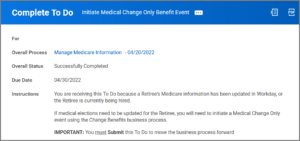
If the Effective Date is 90 OR LESS days, the Change Benefit Elections event will route to the Employee or Retiree to enroll in medical coverage with the option to select the 65+ plan if that is desired. If the Effective Date IS MORE than 90 days in the past, the Change Benefit Elections event will route to the Benefits Partner to enroll the Employee or Retiree in medical coverage with the option to select the 65+ plan if that is desired.
- Return to your inbox to Submit the To Do.
This completes the Managing Medicare Information for Your Employee process.